Physical Exam Template Soap Note
Examination templates for adult males or females. The soapnote project forms notes checklists calculators.
Newborn Exam Physical Template Jonandtracy Co
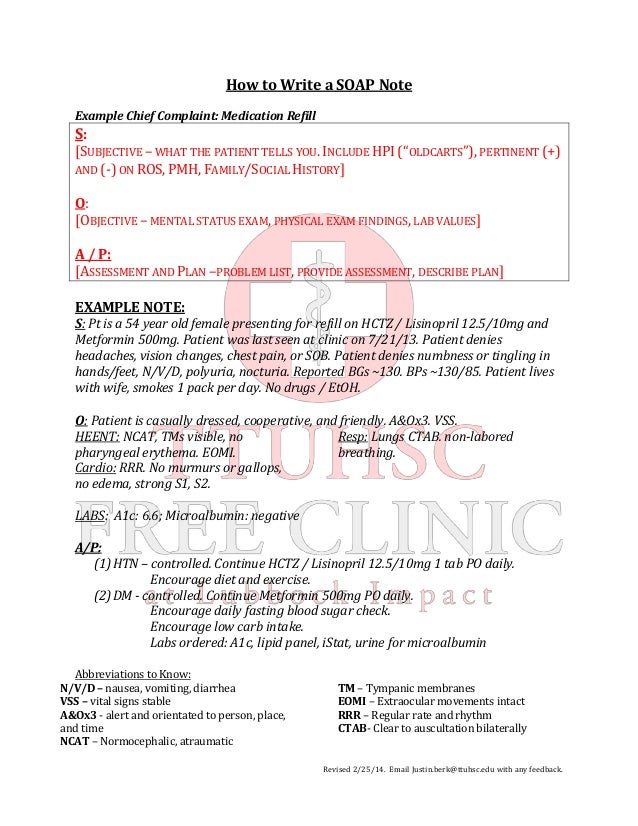
The soap note is an update on an existing problem as in a post op visit or follow up of a problem.
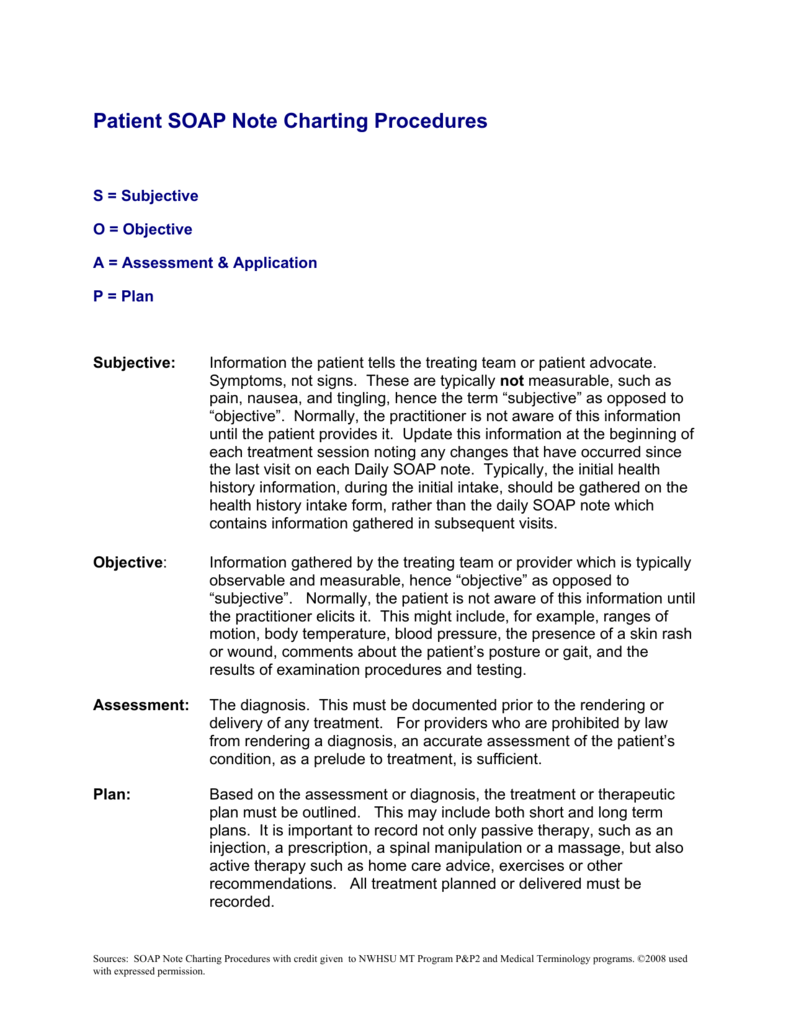
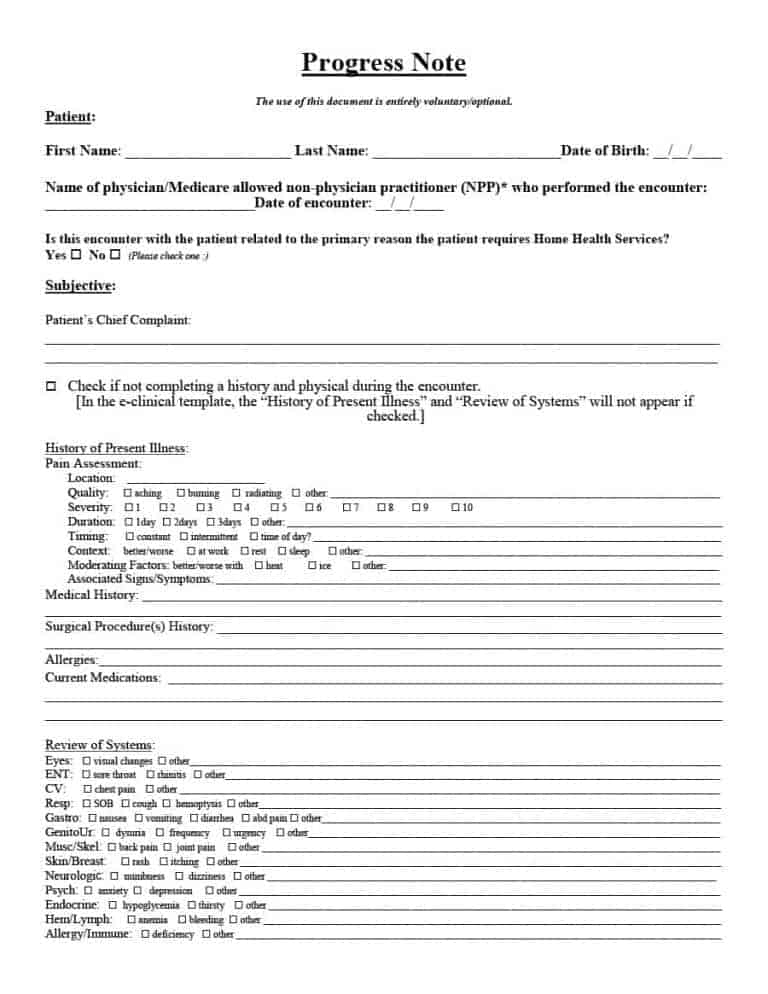
Physical exam template soap note. This format is used in inpatient and outpatient settings and is organized in the subjective objective assessment and plan format that you have been using in year 1 and 2. Subjective the history section. Home education requirementsgrading history and physical examination hp examples.
Complete h p and soap note formats. Ears nose mouth and throat patient denies vertigo headaches sinus problems epistaxis hoarseness dental problems oral lesions hearing loss or changes nasal congestion. Powered by create your own unique website with customizable templates.
Physical exam format 1. In the physical diagnosis course the labs will not generally be a part of the write ups as the chart is not usually available to the students formulation this 83 year old woman with a history of congestive heart failure and coronary artery disease risk factors of hypertension and post menopausal state presents with. Exams for febrile infant fussy infant chicken pox croup and upper respiratory infection.
Normal physical exam template samples. Template for clinical soap note format. Pediatrics complete note featured.
Leg pain medical transcription soap note template. Include symptom dimensions chronological narrative of patients complains. The students have granted permission to have these hps posted on the website as examples.
This is a xx year old female who answers questions appropriately and currently is in no apparent distress. Sample soap note. Vital signs including oxygen saturation when indicated.
Assessment plan elements. Date of last eye exam was august of 2014. Subheadings in all caps and flush left to the margin.
Patient states she does wear contacts. Pe template format 3. Totally free soap notes templates.
Physical exam medical transcription normals. Pediatric health maintenance well child note templates. Her blood pressure is 14274 heart rate is 72 respiratory rate is 22 saturation 98 on room air currently afebrile temperature 982.
History and physical examination hp examples. General adult physical exams. Add to favorites pediatric physical exams.
The links below are to actual hps written by unc students during their inpatient clerkship rotations. The physical exam and laboratory data section.
Writing A Soap Clinic Note Cheat Sheet
Patient Soap Note Charting Procedures
Continuing Medical Implementation Inc
Soap Note Examples For Nurse Practitioners Work Soap
Soap Note Assessment Nursing Template Strand Biology Notes
43 Progress Notes Templates Mental Health Psychotherapy
15 Printable Soap Note Template Forms Fillable Samples In
Free Soap Note Template Documentation Example Writing Format


0 Response to "Physical Exam Template Soap Note"
Post a Comment